Women Are Dying Because Doctors Treat Us Like Men
For years, physicians have referred to women's healthcare as "bikini medicine" and assumed they can diagnose and treat both genders the same way. But it's costing women their lives.


The best day of Starr Mirza's life was the day she went into cardiac arrest. To understand why a then 23-year-old would be overjoyed at a life-threatening condition, one that would require a device to be implanted permanently in her chest, we have to start at the beginning of her medical history.
As a teenager growing up in Lake Los Angeles, a small town an hour outside of L.A., Mirza loved softball, even though she wasn't any good. The running joke among her teammates was that she couldn't make it from first base to second base without falling. "I don't know why they kept me on the team," she says. "I think it was more my spirit than my skill." She didn't know what was wrong with her body, only that she would frequently see stars, hear a ringing sound, feel tingly, and then pass out. When she was a preteen, she went to see a doctor. "I remember it like it was yesterday—I walked in, and right away, I got the eye-rolling," Mirza recalls. "They asked me what I had eaten, if I had issues with my weight, if I had a problem with my brother getting better grades in school than I did. They were trying to say, 'Look, she's doing this for attention.'"
The doctor checked her vitals and sent her home. Her parents took her to get a second opinion, and a third. "By the time we got to the fourth doctor," Mirza, now 37, says, "they were repeatedly saying, 'This is not our problem. You can take her to a psychiatrist and they will deal with her.'"
In the next 20 years, cancer rates will rise nearly six times faster in women than men.
She saw three psychiatrists, all of whom said there was nothing wrong with her mental health. Even her parents had started to doubt her ("They thought I was being a drama queen," Mirza says), so she did her best to live with the mysterious condition, dropping sports, avoiding stairs, and sleeping constantly. Still, she was fainting twice a week, on average, and was in and out of the emergency room up to six times a year. "I wish that just one person would have held my hand and said, 'I believe you—I know you're sick, and we're going to figure this out,'" she says.
After high school, Mirza "avoided doctors like the plague" until that day in 2002 when she went into cardiac arrest. By then, she was 23 and a bank teller in Cape Canaveral, Florida. She was at work when she passed out. When she awoke in a hospital two days later, the doctors told her that her heart had stopped beating and they had placed a cardioverter-defibrillator (a pacemaker and a defibrillator in one) in her chest. Eventually, Mirza was diagnosed with long QT syndrome, a rare heart condition that causes chaotic heartbeats triggering fainting spells and even sudden death. "I started laughing," she says, "because, for 10 years, I knew something was wrong, and finally I was validated."

As Mirza discovered, it can be hard to obtain quality medical treatment as a woman. Studies have shown that female patients' symptoms are less likely to be taken seriously by doctors, and women are more likely to be misdiagnosed, have their symptoms go unrecognized, or be told what they're experiencing is psychosomatic. "It happens all the time," says Dr. Martha Gulati, head of cardiology at the University of Arizona College of Medicine, after hearing the details of Mirza's case. "If you're in health care and take care of a lot of women, you certainly hear these stories and shake your head, because you know what they're going to say, because you see it far too often, unfortunately. The bottom line is, we don't do as good of a job taking care of women as we do men." In the decade Mirza spent waiting for a proper diagnosis, her heart sustained damage that can never be undone. She has had a dozen heart surgeries, went into heart failure in 2013, and will almost assuredly need a transplant one day. "There is inherent bias that makes us undervalue women's symptoms," Gulati adds. "What [Mirza] experienced is a great example of the problem with us not recognizing women at risk—by the time we make a diagnosis, they are living with the consequences of the lack of care."
The best-known incidents of medicine gone wrong in female patients are the many tragic stories of women who died after being sent home from emergency rooms while they were having heart attacks. In fact, a 2000 study published in The New England Journal of Medicine found that women are seven times more likely than men to be misdiagnosed and discharged mid-heart-attack. Most often, that's because doctors fail to recognize women's symptoms, which can differ widely from men's. Only one in eight female heart-attack patients report feeling chest pain, the classic warning sign in men; instead, 71 percent of women have flu-like symptoms. Heart-attack patients who never experience chest pain are nearly twice as likely to die, and in general, women under 50 are twice as likely to die from heart attacks as men of the same age. That could be because even when women—particularly young, healthy women—experience the same symptoms as men, doctors are still more likely to dismiss them.
Stay In The Know
Get exclusive access to fashion and beauty trends, hot-off-the-press celebrity news, and more.
Such was the case for Los Angeles resident Lori Kupetz, who began experiencing "blinding" chest pain in 2005, when she was 38. The cardiologist she saw insisted that her pain was not caused by a heart condition; in the year that followed, she was referred to numerous specialists (gastroenterologists, neurologists) and eventually was told that all she needed was antidepressants. Rather than taking that advice, she made her way to the Cedars-Sinai Women's Heart Center in L.A. (now known as the Barbra Streisand Women's Heart Center), where doctors conducted more specialized tests and found three blocked arteries in her heart—her main aorta was 99 percent blocked—and rushed her into emergency triple-bypass surgery. "I was a walking time bomb," Kupetz says. "Had I listened to the doctor who told me to go on antidepressants, I would not be here today."
"Women are still invisible," Dr. Werbinski says. "We call it: 'Add women and stir.'"
There are also many diseases and conditions that are alarmingly more prevalent among women, and medical science has not discovered why. Women are up to four times more likely to have migraines and chronic fatigue, three times more likely to be diagnosed with autoimmune disorders, and twice as likely to have Alzheimer's, rheumatoid arthritis, and depression. Another puzzling finding: Nonsmoking women are three times more likely to get lung cancer than nonsmoking men, according to a comprehensive 2014 report by Brigham and Women's Hospital in Boston, called "Women's Health Can't Wait." Further, a February 2017 study by Cancer Research U.K. predicts that in the next 20 years, cancer rates will rise nearly six times faster in women than men.
Women of color are at an even greater disadvantage. Black women are twice as likely to have strokes and are much less likely to survive them than white women. They are also more likely to receive the wrong treatment for breast cancer, to be diagnosed at more-advanced stages, to have bigger tumors, and to die. Cardiovascular disease is more common and deadlier in both black and Hispanic women. Hispanic women are also more likely than white women to develop diabetes.
All women are especially at risk when it comes to medications. A 2001 Government Accountability Office report found that eight out of the 10 prescription drugs removed from the market between 1997 and 2000 posed greater health risks for women. Overall, female patients have a 1.5 to 1.7 times higher chance of having an adverse drug reaction. Research suggests that women metabolize drugs differently from men and thus may require distinct doses, yet dosages are rarely broken down by sex. Failing to do so can have disastrous results. In 2013, the Food and Drug Administration (FDA) cut the recommended dose of Ambien and other sleep aids containing zolpidem for women by half after numerous instances of women sleepwalking, sleep-eating, and even sleep-driving—some car accidents were reported—while using the drug.
RELATED STORY

What makes all of this particularly frustrating is that the way female patients are treated isn't an accident—it's by design. Even though science tells us men and women are biologically distinct, medicine largely views us as one and the same. "You think when you are getting care that whether you are a man or a woman is factored into the diagnosis and treatment, but it's often not," says Dr. Janine Clayton, director of the Office of Research on Women's Health at the National Institutes of Health (NIH), the biomedical research facility run by the U.S. Department of Health & Human Services. That's because doctors aren't trained to treat patients that way. Medical schools use curricula informed by what happens in the body of a 154-pound man, and instructors rarely discuss sex differences in their lessons. It's also because, until recently, research was overwhelmingly conducted exclusively on male cells, male mice, and men, and what doctors know about preventing, diagnosing, and treating disease continues to be pulled from such studies. "It was a blind spot," Clayton says. "There hasn't been a really scientific understanding of how important sex is—that this is a basic biological variable that affects us down to the cellular level." The lack of appreciation for sex differences in both education and research is largely to blame for the bias women may face when seeking diagnoses and for the lower-quality care female patients are likely to receive. "Women are not just men with boobs and tubes," says Dr. Janice Werbinski, a gynecologist and executive director of the Sex and Gender Women's Health Collaborative. "We can actually harm women by not researching them correctly and knowing the differences."
Historically, women's health was dubbed "bikini medicine," because medical professionals acted as though the only thing that set women apart were those body parts that could be covered with a bikini. As a result, medical research was rarely conducted on female subjects. In 1977, the FDA recommended excluding female subjects of childbearing age from participating in clinical research (the idea was that researchers risked damaging a fetus if a woman became pregnant during a study). Female mice were also largely excluded because of the misconception that menstrual cycles rendered them too variable to study.
Back then, research findings in men were applied to women without concern that the treatment or drug might not work for them. In 1989, a landmark Harvard University study that found taking aspirin every other day reduced the risk of heart attack by 44 percent in people over age 50 was widely accepted and prescribed in both genders even though it was conducted solely on men ages 40 to 84. (When researchers at Brigham and Women's published its Women's Health Study in 2005, we learned that aspirin does not prevent heart attacks in women under 65 like it does with men.) That was also the heyday for diagnostic guidelines that we now know don't work in women. The "gold standard" test to detect artery blockage, for example, often doesn't reveal plaque in women, as it is more diffuse and harder to see. Similarly, because aortic aneurysms are more prevalent in men, screening guidelines only applied to them, even though aneurysms grow faster and are more likely to rupture in women. At one point, female patients were even much less likely to be placed on kidney-transplant lists because the method doctors used to determine eligibility favored men.
In 1990, the Congressional Caucus for Women's Issues warmed people to the idea that men's and women's bodies are worthy of distinct examination. In August of that year, Senator Barbara Mikulski (D-Maryland) introduced the Women's Health Equity Act, a package of 20 initiatives aimed at improving women's health outcomes and advancing research. It didn't pass, but its existence prompted NIH to create its Office of Research on Women's Health. Three years later, the NIH Revitalization Act was enacted and required that women be considered as participants in research on human subjects. Today, around half of all human subjects in NIH-funded clinical research studies are female.
That should be cause for celebration, but the attempt to fix the gender imbalance in research didn't go far enough. Some key ailments have not received enough focus. An editorial published in the American Heart Association's Circulation journal in 2015 cited reports that show female subjects are "woefully underrepresented" in cardiovascular research, even though heart disease is the number-one killer of women. "I can't overstate the need for sex-specific diagnostic testing and treatments," says Dr. Noel Bairey Merz, medical director at Cedars-Sinai Women's Heart Center. "If you were going to try to do one thing that made a really big difference for women's health, you would crack that nut." In addition, twice as many women than men suffer from depression, yet fewer than 45 percent of studies on the condition use female animals. Similarly, 70 percent of people with chronic pain are women, yet 80 percent of pain studies are conducted on male mice or men. (It's no surprise, then, that men are more likely to be prescribed painkillers; by contrast, women are more likely to be given sedatives.) Drug studies, often funded by pharmaceutical companies, are of particular concern. In 2015, when the FDA approved flibanserin, the so-called female Viagra, it cautioned against drinking while using the pill. Just one problem: The study on the interaction between flibanserin and alcohol was conducted on 25 human subjects—23 of whom were male— even though the drug is prescribed only to women. Even when women are included in studies, researchers often fail to report their findings by sex. Lumping both genders together in the results means there's no way to tell how women fared relative to men. "Women are still invisible," Werbinski says. "We call it: 'Add women and stir.'"
There's also overt sexism to overcome. This is especially true among concussion patients. Women suffer concussions at a higher rate than men, have a larger number of symptoms, and take longer to recover, according to statistics compiled by awareness group Pink Concussions. But most of the research on traumatic brain injury has been done on men, and public awareness of the condition is largely based on the experiences of male football players. Maybe that's why athletic trainers are less likely to recognize concussions in female athletes and why women are less likely to get proper concussion treatment. "My doctors didn't take my injury seriously," says Baltimore resident Alicia Jensen, 20, who experienced severe headaches every day for months after suffering a concussion during a high school soccer game. "I had to convince them of how hard I was hit by the ball—I felt like I had to exaggerate just to make them believe me." What Jensen describes is known in the medical community as "Yentl syndrome," the notion that women have to prove they are as sick as men or have to mirror their symptoms to receive the same level of care. (The term was coined in 1991 by Dr. Bernadine Healy, the late cardiologist and first female head of NIH; she named the syndrome after Yentl, the heroine of a 19th-century short story who disguised herself as a man in order to go to school.)
"I felt like I had to exaggerate just to make them believe me."
NIH is combating such assumptions by incentivizing researchers to take a harder look at women. As of January 2016, in addition to requiring funding applicants to include female human subjects in research trials, the agency now mandates that grantees study both sexes of animals and cells as well, or include a "strong justification" for why they are not. The new guidance also encourages reporting results by sex, and to spur action on that front, Clayton of the NIH's Office of Research on Women's Health says her team is working with medical-journal editors to develop publication standards that will favor studies that do. Many experts are heralding the sex-specific direction NIH is moving in and hoping the agency's status as the nation's largest single public funder of research will inspire others to follow its lead. "NIH funds $33 billion in research a year," says Dr. Marjorie Jenkins, director of medical initiatives and policy advancement in the Office of Women's Health at the FDA, which is also working to address the issue. "When they set the mandate to study both genders, it's a game changer."
Marley Hoggatt, 31, knows the literal pain that can come from doctors who are quick to dismiss female patients. In 2012, while working as a community development specialist for Girl Scouts in Amarillo, Texas, she started getting excruciating migraines two or three times a month. She went to her regular doctor, who asked if she was stressed at work and prescribed an antidepressant. When that didn't work, Hoggatt was referred to a neurologist, who asked about her love life. "He said, 'Well, how is your home life? How is your relationship with your boyfriend?'" Hoggatt remembers. "He recommended a counselor to talk about my 'boy problems.'"
She suffered for two years (often taking "six ibuprofen at once just to try to function") before seeing Dr. Joanna Wilson, an Amarillo-based internist. Wilson ordered an MRI that uncovered one herniated disc and two bulging discs, as well as a pinched nerve, in her neck. "They had been there for years, and no one had bothered to look," Hoggatt says. "I was furious." Wilson referred her to physical therapy, and now she gets one or two migraines a year. "I used to think, Maybe I should just be tougher. So I'd be throwing up on the bathroom floor from the pain, thinking, I should be tougher," Hoggatt says. "When I found out there was an actual physical thing wrong, it was such a relief, because it meant I wasn't just a hypochondriac or a sissy—it was real."
Wilson sees patients like Hoggatt all the time. They often come to her after having seen countless other physicians. "If someone makes the effort of going to doctor after doctor, and all they are given is a pat on the head and told, 'Oh, sweetie, you'll be OK—you just need to smile more,' that is a failure of the physicians," she says. "I will assume the patient has a real disease and do my very best to discover the real physical cause." That makes her somewhat rare among medical professionals. "Unless other doctors have made a concerted effort to reeducate themselves," Wilson says, "they are probably not aware of the majority of sex and gender differences."
RELATED STORY
Hoggatt's experience made it clear to her just how crucial it is to have a doctor who takes women's concerns seriously. These days, she helps design curricula at the Laura W. Bush Institute for Women's Health at Texas Tech University. Since its founding in 2007, the institute has been on the forefront of the push to include sex-specific instruction in medical education. In 2011, it surveyed faculty members at 159 medical schools across the U.S. and Canada. Of the 44 colleges that responded, 70 percent said they had not formally integrated sex differences. "It's the best-kept secret that we are teaching one-sex medicine," says Jenkins, who served as the institute's chief scientific officer before joining the FDA. "We need our students to come out of medical school asking, first and foremost, 'Does sex matter?' and 'Will it make a difference in how I treat my patient?'"
While at Texas Tech, Jenkins and her team developed a curriculum that schools can use to incorporate sex differences into instruction. In 2015, they presented the materials at the first national symposium of gender-based medical education, which was attended by representatives from 111 schools. Ten medical schools, including the Mayo Clinic School of Medicine and Northwestern University, are now using Texas Tech's curriculum. The institute also offers continuing education credits for practicing doctors who want a crash course in sex differences. "I always ask my students," Jenkins says, "'Wouldn't you want your doctor to know the difference?'"
The good news is, a growing number of medical professionals are answering yes to that question. "We now know it's really not good science to apply findings from males to females," says Clayton of NIH's Office of Research on Women's Health. "And we certainly know it's not good medicine to apply anything we learned from a study of only men to women." Luckily, it doesn't always take much to make an impact. When Johns Hopkins Hospital in Baltimore implemented a simple checklist requiring doctors to review blood-clot prevention for every patient, women went from being nearly 50 percent less likely than men to be given blood-clot preventive care to receiving roughly equal care.
Still, medicine moves at a glacial pace—it can take 20 years or more for a scientific discovery to result in a new medication or treatment. Thus, it will likely be decades before advancements made today result in better care for women. In the meantime, women must be their own advocates. "What we're telling women is, every time you go to the doctor, ask, 'Has this treatment or drug been tested on women?'" says Teresa Woodruff, director of Northwestern University's Women's Health Research Institute. "Continue to advocate so physicians have to ask, they have to look it up." She adds, "I think the more people are a little bit outraged, the faster change will occur."
This article appears in the May 2017 issue of Marie Claire, on newsstands now.
Kayla Webley Adler is the Deputy Editor of ELLE magazine. She edits cover stories, profiles, and narrative features on politics, culture, crime, and social trends. Previously, she worked as the Features Director at Marie Claire magazine and as a Staff Writer at TIME magazine.
-
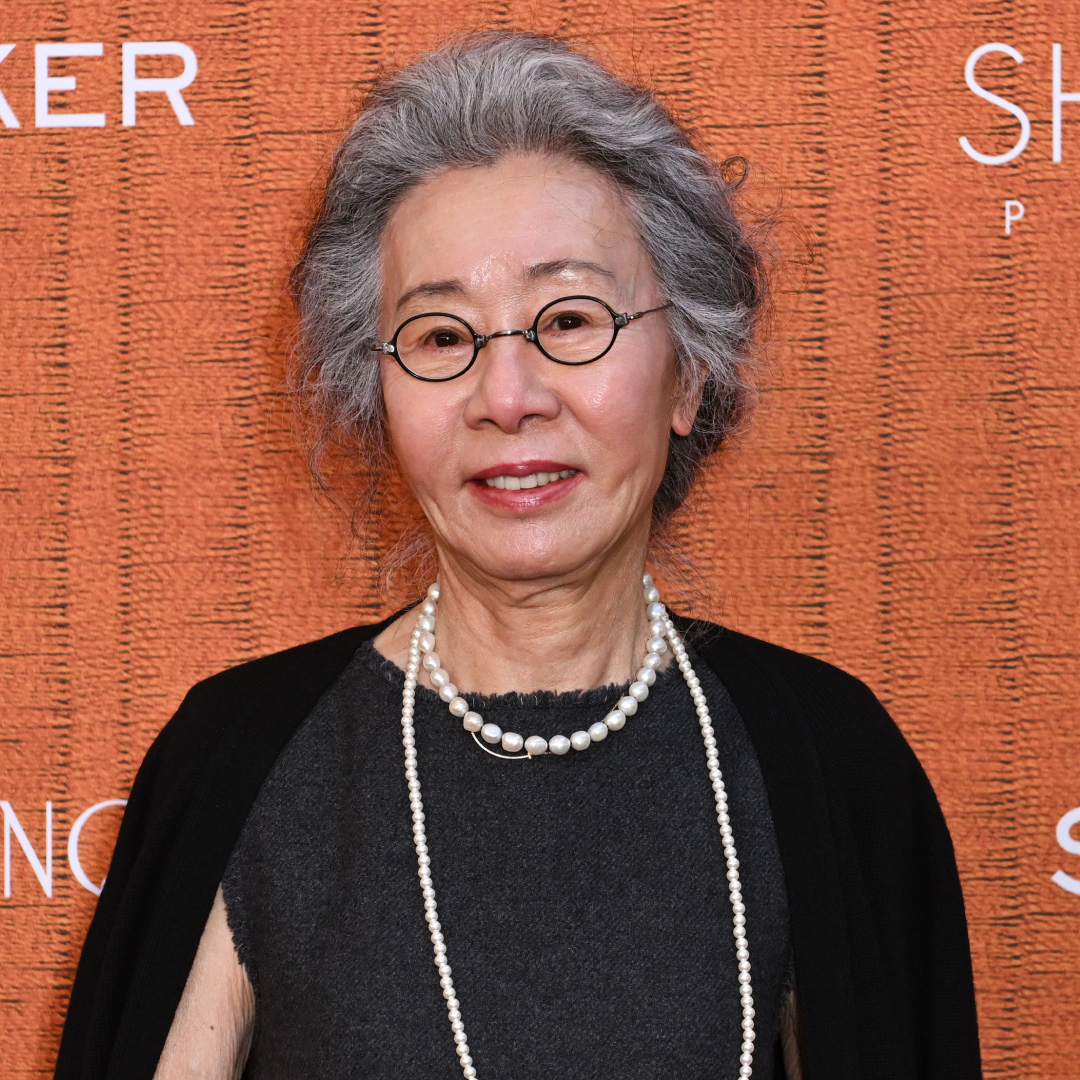 Youn Yuh-Jung Didn't Want to Make Another American Movie—Then Came 'The Wedding Banquet'
Youn Yuh-Jung Didn't Want to Make Another American Movie—Then Came 'The Wedding Banquet'The Oscar winner shares why the LGBTQ+ rom-com hit close to home and the message she hopes it sends to ''conservative'' Koreans.
By Quinci LeGardye
-
 The 17 On-Sale Beauty Finds I’m Stocking Up on Ahead of Summer
The 17 On-Sale Beauty Finds I’m Stocking Up on Ahead of SummerFrom glowy blushes to the all-time best sunscreen.
By Brooke Knappenberger
-
 My Incredibly Picky Mom Told Me Every Beauty Product She Wants for Mother's Day
My Incredibly Picky Mom Told Me Every Beauty Product She Wants for Mother's DayShopping made easy.
By Samantha Holender
-
 I Work Out 5 Days a Week—These Are the Brands I Wear on Repeat
I Work Out 5 Days a Week—These Are the Brands I Wear on RepeatSponsor Content Created With Nordstrom
By Emma Walsh
-
 The Wellness Issue
The Wellness IssueLooking at women's health through a new lens.
By Marie Claire Editors
-
 Senator Klobuchar: "Early Detection Saves Lives. It Saved Mine"
Senator Klobuchar: "Early Detection Saves Lives. It Saved Mine"Senator and breast cancer survivor Amy Klobuchar is encouraging women not to put off preventative care any longer.
By Senator Amy Klobuchar
-
 I'm an Egg Donor. Why Was It So Difficult for Me to Tell People That?
I'm an Egg Donor. Why Was It So Difficult for Me to Tell People That?Much like abortion, surrogacy, and IVF, becoming an egg donor was a reproductive choice that felt unfit for society’s standards of womanhood.
By Lauryn Chamberlain
-
 The 20 Best Probiotics to Keep Your Gut in Check
The 20 Best Probiotics to Keep Your Gut in CheckGut health = wealth.
By Julia Marzovilla
-
 Simone Biles Is Out of the Team Final at the Tokyo Olympics
Simone Biles Is Out of the Team Final at the Tokyo OlympicsShe withdrew from the event due to a medical issue, according to USA Gymnastics.
By Rachel Epstein
-
 The Truth About Thigh Gaps
The Truth About Thigh GapsWe're going to need you to stop right there.
By Kenny Thapoung
-
 The High Price of Living With Chronic Pain
The High Price of Living With Chronic PainThree women open up about how their conditions impact their bodies—and their wallets.
By Alice Oglethorpe