Fungal Acne: The Causes and Treatments, According to Dermatologists
Turns out, fungal acne isn't actually acne at all.


Show me your pimple and chances are I can tell you exactly what type of acne you’re dealing with and how to treat it. I’m a skincare nerd and this is one of my beauty editor superpowers. While blackheads, whiteheads, and even cysts are pretty easy to identify when you know what to look for, fungal acne can be a little, ok a lot, trickier. It basically majored in deception and, if I’m being completely honest with you, it’s not actually acne at all. “It looks the same, but instead of traditional acne, or folliculitis, which is caused by bacteria, fungal acne is caused by a type of fungus called yeast,” explains board-certified dermatologist Dr. Sheila Farhang.
That in mind, traditional acne treatments aren’t going to cut it. The best spot treatment in the world will do next to nothing. Instead, you’re going to want to pop over to your drugstore’s hair care aisle (we’ll explain why below, fear not), make a few lifestyle changes, and pay a visit to your derm, ASAP. To get more info on how to diagnose fungal acne, learn what causes it, and get some tips on how to treat it from the pros themselves, scroll ahead.
What Is Fungal Acne?
Not to burst your bubble, but fungal acne is kind of fake news. “It’s a misnomer and not a medical term that dermatologists use,” says board-certified dermatologist Dr. Lindsey Zubritsky. “The correct medical term is pityrosporum folliculitis and it’s not acne at all.” Think of it this way: Acne vulgaris, aka your whiteheads, blackheads, cysts, papules, and pustules, is typically caused by either dead skin cells, bacteria, excess oil, clogged pores, inflammation, or hormones. Traditional folliculitis is the result of bacteria. Fungal acne on the other hand is caused by a type of yeast (it’s called M. furfur in case you were wondering) rooted on the hair follicle. “This is very similar to what causes dandruff,” adds Dr. Farhang. As such, fungal acne is going to feel a heck of a lot more itchy than a traditional breakout.
What Does Fungal Acne Look Like?
Fungal acne can look pretty damn similar to a papule or pustule, but there are some key differences. “Fungal acne tends to be less inflammatory and not cystic—just little tiny bumps that are either skin colored or pink,” says Dr. Farhang. Location is also going to be a huge factor. While acne vulgaris is mainly going to pop up on your T-zone, chin, jawline, and neck, the small red-ish bumps associated with fungal acne have a different happy place. “Typical locations include the upper chest, upper to mid back, temples, sides of the face, hairline, and forehead,” says Dr. Zubritsky.
What Causes Fungal Acne?
Before you get ahead of yourself and freak out about having a fungus on your face or body, take a deep breath. Almost every single person has some degree of fungus living on their skin. It’s normal! That fungus turns into fungal acne, or fungal folliculitus, when the yeast goes into overdrive and makes its way into the hair follicle. This can happen for a few reasons.
One of the most common? Antibiotics or oral steroids, like prednisone. Now don't get me wrong, some antibiotics, like doxycycline for example, can result in an *amazing* skin day. But the reverse holds true too. “Antibiotics can cause an imbalance. When the bad and good bacteria is gone, it can cause yeast to overproduce,” explains Dr. Farhang. “This is similar to why some people get vaginal yeast infections after taking oral antibiotics. All the bacteria that typically keeps the fungus regulated is MIA and it becomes a bit of a free for all.
If antibiotics haven’t been in the picture, your yeast imbalance is likely being made worse by trapped moisture that allows the fungus to breed at a more rapid rate. Think: The sweat that hangs out on your body post-workout. “Fungal acne is exacerbated by warm, humid, and moist conditions,” says Dr. Zubritsky, noting that it spikes more in the summer months.
Stay In The Know
Get exclusive access to fashion and beauty trends, hot-off-the-press celebrity news, and more.
It’s also possible that you’re predisposed to developing fungal acne, namely if you have an autoimmune disease.
How to Treat Fungal Acne
There are certainly some at-home or over-the-counter remedies that can help reduce fungal acne, but it’s always best to consult with your board-certified dermatologist beforehand. Since fungal acne can be tricky to diagnose, they may want to take a culture to confirm what you’re dealing with ahead of treatment.
Try an Anti-Dandruff Product
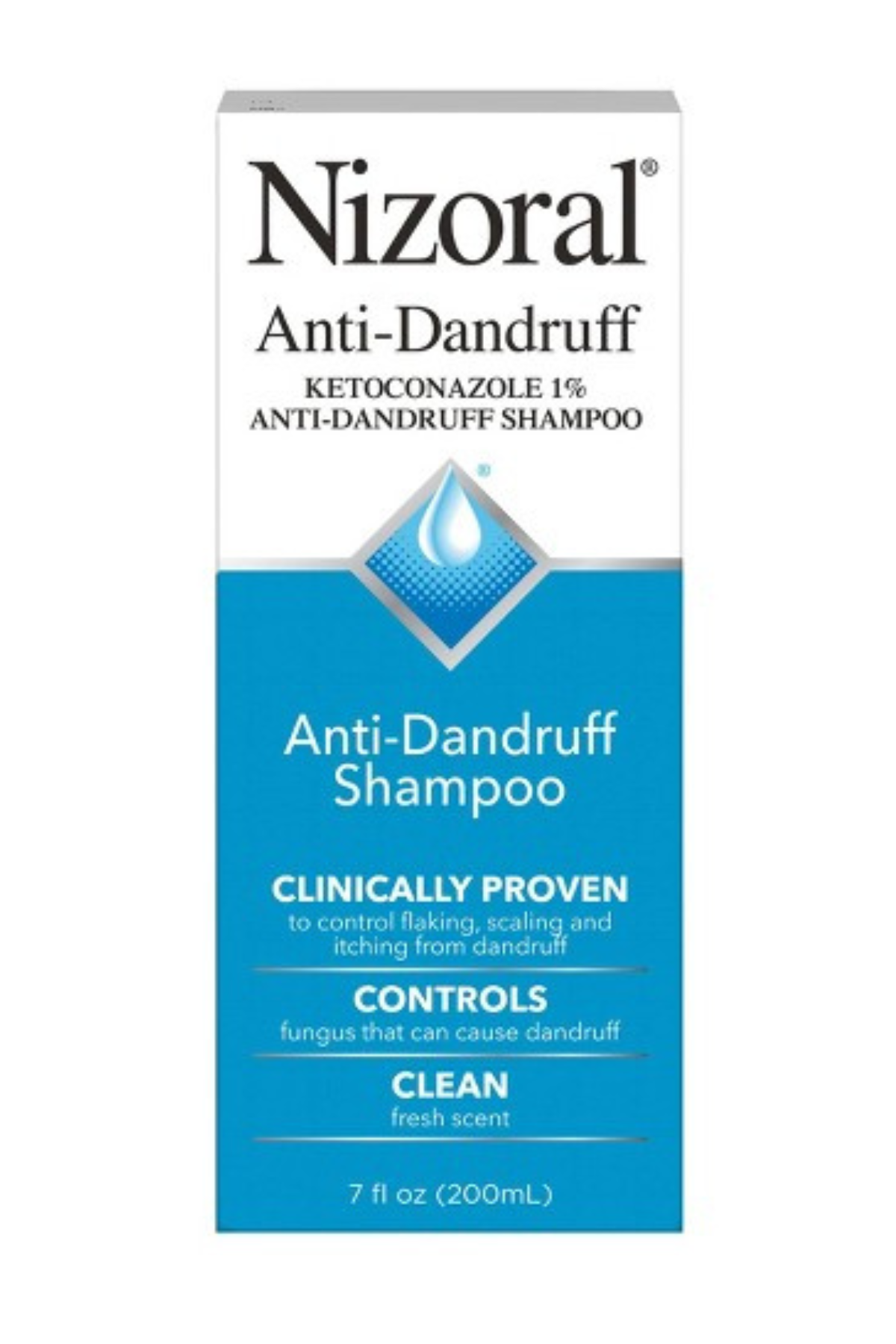
Because the type of yeast responsible for fungal is very similar to the type of yeast responsible for dandruff, it shouldn’t come as too much of a shocker that the treatments align. “Over the counter, anti-dandruff or anti-fungal shampoos work well for this condition,” says Dr. Zubritsky. “It’s best to apply these shampoos to the affected areas, let them sit for 10 minutes, and then rinse them off in the shower. Use it several times a week for best results.”
You’re going to want to pick a product with an INCI that contains zinc pyrithione, selenium sulfide, or ketoconazole. And before you ask: Yes, these are a-ok to use on your face.
Shower After Sweating
This is perhaps one of the easiest changes you can make to your routine—it’s a no harm, no foul option. “It’s best to avoid any habit that traps dirt or sweat on the skin,” says Dr. Zubritsky. “For example, after working out or sweating heavily, it’s best to immediately rinse your skin or shower and change out of your sweaty clothes.”
If hopping in the shower isn’t an option or you tend to get sweaty while just living your life, carry some cleansing wipes around with you for a quick fix. While it’s by no means as good as a straight up shower, it can remove some of that moisture and dirt buildup.
Avoid Heavy Skincare
While fungal acne might have the word “acne” in its name, it needs to be treated wayyyy differently than run-of-the-mill breakouts. Unfortunately acne treatments can actually make matters worse. “They can disrupt the skin’s microbiome and lead to yeast overgrowth,” explains Dr. Zubritsky. She also suggests steering clear of heavy sunscreens, moisturizers, or makeup, as they can end up clogging pores and hair follicles, which in turn, makes fungal acne flare even more. Stick to lightweight, water-based, non-comedogenic products.
See Your Doctor
“If you suspect you have fungal acne, I recommend seeking help from your dermatologist from the gate,” advises Dr. Zubritsky. “It can be extremely difficult to differentiate fungal acne from bacterial folliculitis from acne vulgaris.” Your dermatologist may recommend over-the-counter products following a proper diagnosis, but it’s also possible they’ll want to write you a script for a stronger prescription topical or oral antifungal.
Meet the Dermatologists

Lindsey Zubritsky, MD, FAAD, is a board-certified dermatologist specializing in general medical dermatology, surgical dermatology, cosmetics, and pediatric dermatology. Originally from Pittsburgh, Pennsylvania, she graduated summa cum laude from Washington and Jefferson College in Washington, PA with a degree in Cell/Molecular Biology where she participated in collegiate soccer. She was inducted into Phi Beta Kappa, the oldest and most prestigious academic honor society in the United States. She then completed her medical school training at Penn State College of Medicine in Hershey, PA where she graduated at the top of her class and was inducted into the esteemed Alpha Omega Alpha Honor Medical Society. She completed a year of internal medicine training during her transitional year at Kettering Medical Center in Dayton, Ohio. She then pursued her residency in dermatology at the University of Cincinnati Medical Center where she served as chief resident. She is passionate about all things dermatology, especially debunking skincare myths and educating the public using her social media platforms. She is a Fellow of the American Academy of Dermatology and serves as one of their social media ambassadors. She is also an editor for the Journal of the American Academy of Dermatology (JAAD), the leading evidence-based peer-reviewed medical journal for dermatologists, and routinely reviews submissions for publication. She has contributed to numerous beauty articles as a skincare and dermatologic expert including Women's Health, Byrdie, InStyle magazine, Forbes, CNN, MSN, Esquire magazine, BuzzFeed, Allure, Yahoo!, The EveryGirl and many more. She has lectured at several national and local conferences and was the guest speaker for Grand Rounds at numerous dermatology residency programs across the country. Dr. Zubritsky utilizes her skills to optimize patient care and strives to form personal connections with her patients in order to build a strong, trusting relationship. She is thrilled to be providing dermatological care on the Mississippi gulf coast and surrounding areas at Premier Dermatology and Skin Cancer Center.

Dr. Sheila Farhang is a board-certified dermatologist and double-fellowship trained cosmetic surgeon as well as a reconstructive Mohs micrographic (skin cancer) surgeon. “Dr. Sheila” as many know her as, stands out in the dermatology space as she has expertise in both integrative skincare and cutting-edge procedures. She is also highly regarded in the female empowerment space being a founder, CEO, and multi-business owner. Dr. Sheila attended the University of Texas for her undergraduate and medical degrees. Dr. Sheila then completed her dermatology residency at the University of South Florida Department of Dermatology and Cutaneous Surgery. During this time, she augmented her surgical education with additional training with plastic surgeons. Upon completion, she was selected for a position at arguably one of the most competitive programs in the country for dual fellowship at the Skin Institute of South Florida and Hollywood Dermatology in the Miami, FL area. During this time, she also completed a year-long entrepreneur and leadership program through the Advancing Innovation in Dermatology led by Harvard faculty and international industry leaders.

Samantha Holender is the Senior Beauty Editor at Marie Claire, where she reports on the best new launches, dives into the science behind skincare, and shares the breakdown on the latest and greatest trends in the beauty space. She's studied up on every ingredient you'll find on INCI list and is constantly in search of the world's glowiest makeup products. She's constantly tracking the biggest nail and hair trends to pop up in the beauty space, going backstage during fashion weeks, tracking celebrity looks, and constantly talking to celebrity hair stylists, nail artists, and makeup artists. Prior to joining the team, she worked as Us Weekly’s Beauty and Style Editor, where she stayed on the pulse of pop culture and broke down celebrity beauty routines, hair transformations, and red carpet looks. Her words have also appeared on Popsugar, Makeup.com, Skincare.com, Delish.com, and Philadelphia Wedding. Samantha also serves as a board member for the American Society of Magazine Editors (ASME). She first joined the organization in 2018, when she worked as an editorial intern at Food Network Magazine and Pioneer Woman Magazine. Samantha has a degree in Journalism and Mass Communications from The George Washington University’s School of Media and Public Affairs. While at GWU, she was a founding member of the school’s HerCampus chapter and served as its President for four years. When she’s not deep in the beauty closet or swatching eyeshadows, you can find her obsessing over Real Housewives and all things Bravo. Keep up with her on Instagram @samholender.
-
 Rico Nasty Shares What Music Shaped Her—and What's on Her Playlist Now
Rico Nasty Shares What Music Shaped Her—and What's on Her Playlist NowWith her new album 'LETHAL' coming soon, the rapper opens up about her musical preferences for the 'Marie Claire' series "Listen Up."
By Sadie Bell
-
 The Future Queen of the Netherlands Wore the Same Tiara She Used to Play Dress-Up In as a Child
The Future Queen of the Netherlands Wore the Same Tiara She Used to Play Dress-Up In as a ChildIt was a full-circle moment for Princess Catharina-Amalia, who admits, "I love tiaras."
By Kristin Contino
-
 Monica Barbaro Makes a Velvet Bath Robe Feel Couture
Monica Barbaro Makes a Velvet Bath Robe Feel CoutureOnly for Dior's front row.
By Kelsey Stiegman