I Was Betrayed by a Pill
The abortion pill was supposed to make termination safe, easy, and discreet. One pro-choice advocate found it anything but.
From the moment it was approved in 2000, I believed in the abortion pill. I thought, Finally! Abortion would at last become what it always should have been: a private medical matter between a woman and her doctor. It held the promise of a swift, at-home termination. There would be no more gauntlets of protesters at clinics, because who would know which physicians were dispensing the pills? Even better, the pill would keep abortion accessible at a time when fewer gynecologists were willing to perform them out of fear of attacks.
Nonetheless, I never expected I'd need to consider using it myself. I had just been at my gyno discussing fertility options. Stewart and I were getting married, and we planned to try for a baby right after the wedding. At 38, I was supremely aware that my window of opportunity was closing. Little did I know, lying there with my feet in the stirrups, pondering whether I ought to freeze my eggs in case we had trouble conceiving later, that I was already pregnant; it was too early to detect with a pelvic exam. But four weeks later, as I stared at the double pink lines (I took three tests to be sure), the facts were undeniable.
I should have been elated. Instead, I was distraught. This was not how things were supposed to go. My concern was about more than tossing middle-class conventionality-wedding first, family second-out the window. At the time, Stewart and I were living in Las Vegas, land of the all-night-and-way-into-the-next-morning party. In order to work all day and party, party, party all night, I'd been relying on a cocktail of caffeine and Peruvian marching powder. When I backtracked through my calendar, I realized I'd gotten pregnant when I was, shall we say . . . marching almost daily.
Stupid! Stupid! Stupid! I cursed myself as I drove home from the Walgreens where I'd bought the third test, hoping against hope that there had been a mistake with the other two. I was so impatient for the results, I ripped open the package in the store bathroom and peed on the wand right there. Oh, I was pregnant all right. How could I have been so irresponsible? You start a pregnancy with a healthy diet and prenatal vitamins, not cocaine-I didn't have to consult a panel of experts to know that. No matter what I did from this point on, there would always be the chance that the baby would have problems-maybe physical ones, maybe psychological issues. I wasn't willing to roll the dice with another life. I could really see only one option. I broke the news to Stewart in one breath: I'm pregnant, and we need to abort.
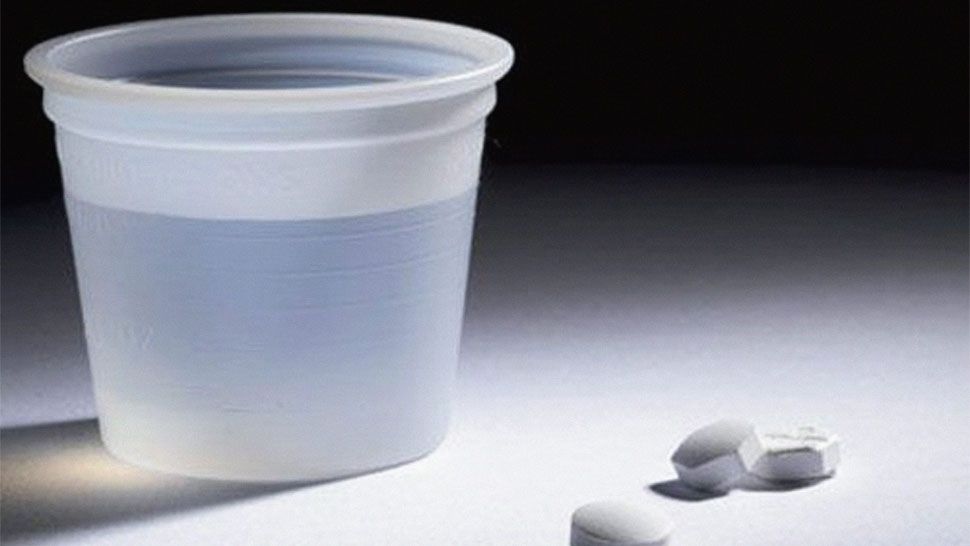
He didn't need any convincing. The next question was how to abort. There was the surgical option, of course. I'd had one in college (so you'd think I would have learned this lesson already), and I dreaded the needle that would be used to numb my cervix. In the years since college, another option had emerged: A pill called mifepristone (formerly RU-486, now sold under the brand name Mifeprex) could trigger what experts call a "medical abortion." Mifepristone isn't to be confused with Plan B, the "morning after" pill that can prevent pregnancy if you take it within 72 hours of unprotected sex.
This one (also called the "early option" or the "abortion pill") is used together with the synthetic hormone misoprostol to abort when you're already pregnant. First, mifepristone blocks the action of progesterone, the hormone that's needed to sustain pregnancy. Then, misoprostol empties the uterus. The Mifeprex literature described some cramping and bleeding, "similar to or greater than a normal, heavy period." This sounded far more appealing than surgical abortion. A few pills, a couple of cramps, and it would all be over. We could move on with our lives.
But as it turned out, things weren't quite that simple.
Stay In The Know
Get exclusive access to fashion and beauty trends, hot-off-the-press celebrity news, and more.
For starters, the abortion pill is not always easy to get. In Nevada, where the state constitution guarantees the right to abortion, my own gynecologist refused to administer the pill-not because he's antiabortion, but, he explained, somewhat apologetically, just as he didn't do surgical abortions because he feared becoming a target of abortion foes, he didn't do medical abortions, either. Nor would he simply write me a prescription and let me do it myself. "They watch what I prescribe at the pharmacy," he told me. So much for discretion and accessibility.
Fortunately, after searching online, I was able to find a cooperative local clinic. The initial procedure was simple enough. I had an ultrasound to confirm that the pregnancy wasn't lodged in the fallopian tubes (a case where Mifeprex can't be used). I signed a release stating that I understood how the drug worked and all the risks involved. Then I downed the Mifeprex and went home. Two days later, it was time for the misoprostol. This part I could do at home. Clinic staffers had directed me to insert the tablets into my vagina in the morning so I'd have the day to recover. I envisioned recuperating on the couch with some uncomfortable but bearable cramps and soothing myself with bad daytime TV. I kissed Stewart good-bye. He said he'd call later. I went to insert the tablets.
I never made it to the couch.
Nothing-not the drug literature, not the clinic doctor, not even my own gyno-had prepared me for the searing, gripping, squeezing pain that ripped through my belly 30 minutes later. I couldn't even form words when Stewart called to check on me. It was all I could do to gasp, "Come home! Now!" For 90 minutes, I was disoriented, nauseated, and, between crushing waves of contractions that I imagine were close to what labor feels like, racing from the bed to the bathroom with diarrhea. Then, just as quickly, it was over. The next night, I started bleeding. I bled for 14 days. A follow-up ultrasound confirmed I'd aborted. And that's when my problems really began.
I had been prepared for the possibility that the pill wouldn't work and I'd still need a sur-gical abortion-that happens in about 5 to 8 percent of cases. I also knew that I might bleed so heavily I'd need surgery to stop it-about 1 percent of women do. What blindsided me, apart from being battered by the misoprostol, were the huge cystic boils that soon covered my neck, shoulders, and back. I was also overcome by fatigue-an utter lack of ability to do anything more strenuous than sleep or lie on the couch. My brain felt so fuzzy, English seemed like a second language, and I couldn't work. On top of all that came depression: I sobbed constantly. I wouldn't leave the house. I stopped showering.
It was only after I described my symptoms to my gynecologist that I discovered my experience wasn't all that unusual. (The Mifeprex literature didn't even mention it.) "I think it's underreported, but probably one in three women have dramatic side effects," he told me. My body was in hormonal chaos-pregnancy hormones clashing with antipregnancy hormones clashing with stress hormones. "I've seen a lot of women go through-I don't want to call it postpartum, but postevent-melancholy that's more dramatic than people want to admit," he said. He prescribed antidepressants. "One day, you'll feel just like your old self." It took nine months.
I'm very reluctant to give antiabortion advocates any more tools for chipping away at our right to safe, legal, accessible abortions. And despite my experience, I'm not suggesting the abortion pill be banned. (Viagra carries a higher risk of death, and no one's calling for a ban on that.) But I am bitterly disappointed that it's not the panacea millions of women like me thought it would be.
It doesn't help that those who dispense mifepristone/misoprostol don't always know as much about the drugs as they should. In fact, at the clinic I visited, the doctor couldn't tell me which hormone the combination used.
Much later, I also learned about several deaths linked to the abortion pill. In one case, it was given to a woman who never should have received it-she had an undiagnosed ectopic pregnancy and died from associated hemorrhaging. But five other women developed mysterious, fatal bacterial infections. Reading about them, my stomach twisted. I'd used the pills exactly as they had. I couldn't help but wonder: Could I have died?
The drug's manufacturer and the FDA have emphasized that a "causal relationship" between the pills and the infection that reportedly killed these women hasn't been established. And given that the rare bacterium, Clostridium sordellii, responsible for the deaths has killed a handful of other people-including a man undergoing surgery-it seems likely that more than just the pills are responsible.
The scary thing is that no one knows what. It's possible that together, the abortion pill and pregnancy suppress immune function enough to make some women more vulnerable to infection. There's also been some suggestion that inserting misoprostol into the vagina might raise the risk of infection. (Although the FDA approved it for oral use, many clinics instruct women to use it vaginally because research shows that the process works just as well but with fewer side effects.) But gynos like Anne Davis, M.D., M.P.H., assistant professor of obstetrics and gynecology at Columbia Presbyterian Medical Center in New York City, pooh-pooh that theory. "Literally hundreds of thousands of women have used it that way. It seems unlikely that a particular woman putting her fingers in her vagina would give herself an infection."
For the moment, we really don't know whether medical abortion carries any greater risk for infection than, say, surgical abortion, miscarriage, or childbirth. Still, to be safe, Planned Parenthood now instructs women to take misoprostol orally. In addition, Mifeprex now carries a black-box warning about the potential risk for excessive bleeding and serious, even fatal, infection. And because C. sordellii infection mimics the process of medical abortion, the FDA also issued a public-health advisory in July 2005 cautioning women and doctors to look out for prolonged nausea, vomiting, diarrhea, weakness, or abdominal pain (even in the absence of fever) in the days after taking misoprostol. (In the U.K., doctors can look for it themselves: Women stay in the hospital after the pills are administered.)
Of course, these are all good steps toward safeguarding women's health. But you know what else would help? If doctors and clinic staff dispelled the misconception many women have that the "early option" is an easy option. In all fairness, my postabortion experience was, according to several gynecologists, more severe than most. It's entirely possible that the aftershocks I suffered were magnified by grief as well as guilt that I'd brought this on myself. But was it the abortion pill that magnified my grief and guilt over ending the pregnancy or the grief and guilt that magnified my reaction to the abortion pill? There's no way to really know.
To date, about 650,000 women in the U.S. have used the abortion pill, and I'm sure many more will, since the medical literature is filled with reports of satisfied customers. And yet, the questions about what role (if any) the abortion pill played in those fatal infections underscores why it's important to keep surgical abortion accessible.
One gynecologist I talked to not long ago confided that she'd absolutely choose surgical abortion over a medical one, because even without the specter of septic shock, the abortion pill can be, as she put it, "a real ordeal." "We could have told you it wasn't going to be easy," a clinic staffer noted when I rattled off my complaints during my follow-up.
Why didn't she speak up sooner?
-
 Why Duchess Sophie Allegedly Feels "Snubbed" by King Charles
Why Duchess Sophie Allegedly Feels "Snubbed" by King Charles"There should be an opportunity for Sophie to be allowed to do more," a royal expert claimed.
By Amy Mackelden Published
-
 Dua Lipa Swaps Her Valentino Dress for a Marni Mini Skirt
Dua Lipa Swaps Her Valentino Dress for a Marni Mini SkirtThe singer accessorized her outfits with more than $120,000 of jewelry.
By Amy Mackelden Published
-
 Harry Was Allegedly Crushed When William Received "Special Treatment"
Harry Was Allegedly Crushed When William Received "Special Treatment""Poor Harry's face across the table," Princess Diana's former butler recalled.
By Amy Mackelden Published
-
 The All-Time Favorite Sex Positions of 11 Real Women
The All-Time Favorite Sex Positions of 11 Real WomenFeatures "It makes me feel like the sexiest woman on earth."
By The Editors Published
-
 The 22 Best Vibrators, According to Sex Toy Experts
The 22 Best Vibrators, According to Sex Toy ExpertsThe vibes are immaculate.
By Gabrielle Ulubay Last updated
-
 The 20 Best Sex Games for Couples in 2023
The 20 Best Sex Games for Couples in 2023Who said game nights need to be wholesome?
By Gabrielle Ulubay Last updated
-
 The 14 Best Lubes for Every Need
The 14 Best Lubes for Every NeedGood sex should always go smoothly.
By Gabrielle Ulubay Last updated
-
 30 Female-Friendly Porn Websites for Any Mood
30 Female-Friendly Porn Websites for Any MoodFeatures All the best websites, right this way.
By Kayleigh Roberts Published
-
 The 82 Best Cheap Date Ideas for Couples on a Budget
The 82 Best Cheap Date Ideas for Couples on a Budget"Love don't cost a thing." —J.Lo
By The Editors Last updated
-
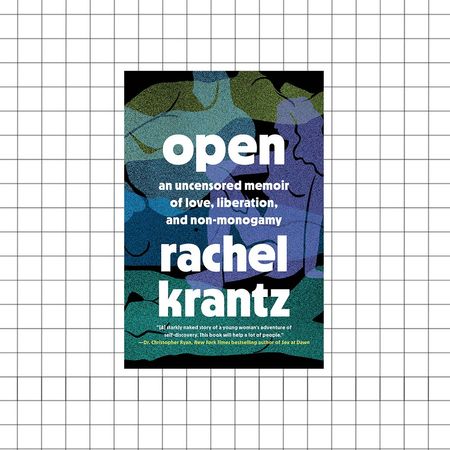 Diary of a Non-Monogamist
Diary of a Non-MonogamistRachel Krantz, author of the new book 'Open,' shares the ups and downs of her journey into the world of open relationships.
By Abigail Pesta Published
-
 COVID Forced My Polyamorous Marriage to Become Monogamous
COVID Forced My Polyamorous Marriage to Become MonogamousFor Melanie LaForce, pandemic-induced social distancing guidelines meant she could no longer see men outside of her marriage. But monogamy didn't just change her relationship with her husband—it changed her relationship with herself.
By Melanie LaForce Published